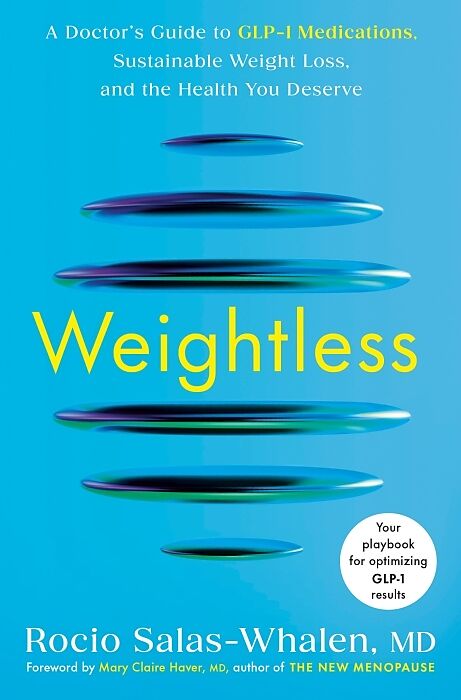
Weightless
Beschreibung
A board-certified endocrinologist shares her must-have guide to using GLP-1 medications, such as Ozempic, Wegovy, Mounjaro, and Zepbound, to reverse obesity and take charge of your health, with established strategies for maximizing your results GLP-1 medicatio...Format auswählen
- Fester EinbandCHF 30.30
Wird oft zusammen gekauft
Andere Kunden kauften auch
Beschreibung
A board-certified endocrinologist shares her must-have guide to using GLP-1 medications, such as Ozempic, Wegovy, Mounjaro, and Zepbound, to reverse obesity and take charge of your health, with established strategies for maximizing your results GLP-1 medications have revolutionized how doctors treat obesity and changed the lives of the people who take them. With demand for these transformative drugs skyrocketing, people interested in trying GLP-1 therapy for weight loss must navigate an uncharted landscape where many doctors are playing catch-up on the latest science. Many patients walk out their doctor’s offices with a prescription but not the essential guidance they need to get the best results--or sustain them. In Comprehensive and research-backed, <Weightless <will give you the science, clarity, and confidence to take the first step toward a healthier, more empowered you.
Autorentext
Rocio Salas-Whalen, MD, is a board-certified endocrinologist specializing in obesity medicine. A recognized leader in the treatment of obesity, perimenopause, and menopause, she is known for integrating cutting-edge therapies—such as GLP-1 medications—into compassionate, personalized care. Originally from Mexico, Dr. Salas-Whalen immigrated to the United States to pursue her dream of becoming a physician. Today, she leads a thriving private practice in New York City. A sought-after expert in both English- and Spanish-language media, she has been featured on The Mel Robbins Podcast, UnaVision, and more.
Leseprobe
Chapter 1
Rethinking Obesity: What We Got Wrong
There is one patient consultation that has stayed with me over the years. The patient was fifty-one years old, successful in his career, polite, thoughtful—and clearly uneasy the moment he stepped into my office. When I asked what had brought him in, he explained that he had tried everything: dieting, fasting, overexercising. He had lost weight many times but always gained it back. He said, “I guess I’m just not trying hard enough, but I just don’t know what else to do.”
I shook my head and told him, “Obesity is not your fault.”
I explained what we now understand about obesity: that it’s not just about what you eat or how much you move; it’s about hormones, genetics, the brain, the gut, and many other factors outside of willpower. And then something unexpected happened. There was a visible shift; I watched the tension in his shoulders ease as his emotional burden was lifted. He started to cry. For the first time, he heard that he hadn’t failed. He felt the validation that what he was up against wasn’t a personal flaw but a medical condition.
And I hadn’t even told him the best part yet: There was something we could do about it.
When I see a reaction like that, it makes me want to share everything I’ve learned about obesity with everyone—and repeat it over and over. In this chapter, you’ll learn what’s going on “behind the scenes of the body” and the reasons behind weight gain in cases like my patient’s—and maybe yours, even if you don’t identify with the term obesity.
Whether or not you’ve been formally diagnosed with obesity, this is a crucial chapter to help you understand your body and its treatment in a whole new way. If you’re someone with excess weight who is considering taking GLP-1 medication—or even just trying to better understand why your body holds on to weight despite all your efforts—read on.
In the pages ahead, we’ll pull back the curtain on what obesity actually is: not a character flaw but a disease influenced by many aspects of our biology and environment. I share this information not to lecture you but to make your experience with GLP-1 therapy more effective, more comprehensive, and ultimately more empowering. I want you to understand that this treatment is informed by real people and real life. Along the way, you’ll also begin to see the full picture of obesity—one grounded in science, not bias.
There’s much to learn ahead, but just as important, there’s much to unlearn.
Understanding Obesity
In medicine, there is a commonly accepted idea that within the patient/doctor dynamic, it is only the patient who needs to learn. This couldn’t be further from the truth, and I am proof of this. In my opinion, a physician who is not learning is a physician who is not listening to their patients.
For decades, medical professionals have been taught to approach obesity as a simple math problem: Eat less, exercise more. This advice was repeated in exam rooms, public health campaigns, and weight loss programs. And because it was presented as a straightforward solution, it also carried an unspoken assumption: If a patient wasn’t losing weight, it must have been due to a lack of effort, discipline, or willpower.
But if this approach truly worked, why did obesity rates continue to rise? Why do millions of people—many of whom have followed every diet, exercise plan, and medical recommendation—still find themselves struggling with their weight? The answer: It’s not because patients aren’t trying but because this approach to treating obesity is fundamentally flawed.
To fully grasp the scope of this issue, let’s step back and examine the bigger picture. The statistics on obesity tell a story—one that makes it clear that obesity isn’t just a personal challenge but a global public health emergency.
The Landscape of Obesity: A Global and National Crisis
Obesity is defined as the abnormal or excessive expansion of adipose tissue. It is a complex disease that affects nearly half of all U.S. adults, and its prevalence is increasing worldwide.
According to the World Health Organization (WHO), worldwide obesity rates have nearly tripled since 1975. Nearly every developed nation has experienced an increase in obesity prevalence. The United States has been at the forefront of this crisis; I’m sure it’s no surprise to you that our obesity rate has been rising at an alarming pace. In 1962, only 13 percent of U.S. adults were classified as having obesity. By 1999, that number had skyrocketed to 30.5 percent. By 2020, obesity affected 41.9 percent of U.S. adults. And today, nearly one in five children in the United States lives with obesity.
At the current trajectory, nearly half of U.S. adults will be classified as having obesity in the next decade. But this is not just an American problem; it’s a global phenomenon. Countries around the world, from the United Kingdom to China, are experiencing rising obesity rates.
What changed? Just a few generations ago, obesity was far less common. People moved more, food was less processed, and portion sizes were smaller. But today’s world looks different. The rise of ultraprocessed foods has made calorie-dense, nutrient-poor options more accessible and affordable than ever before. Sedentary lifestyles have become the norm, with more jobs shifting to office work and many people working remotely. Cities are designed for cars instead of pedestrians, and there are fewer opportunities for physical activity built into daily life. Stress, poor sleep, and environmental factors have contributed to weight gain in ways that weren’t as prevalent in previous generations. The result? A public health crisis that affects every aspect of society.
Obesity is not just about physical appearance or weight; it is directly linked to serious chronic diseases. Individuals with obesity are at higher risk of developing type 2 diabetes, heart disease, stroke, and more than thirteen obesity-related cancers. Because it increases the risk of these diseases, it can shorten lifespan significantly, maki…
