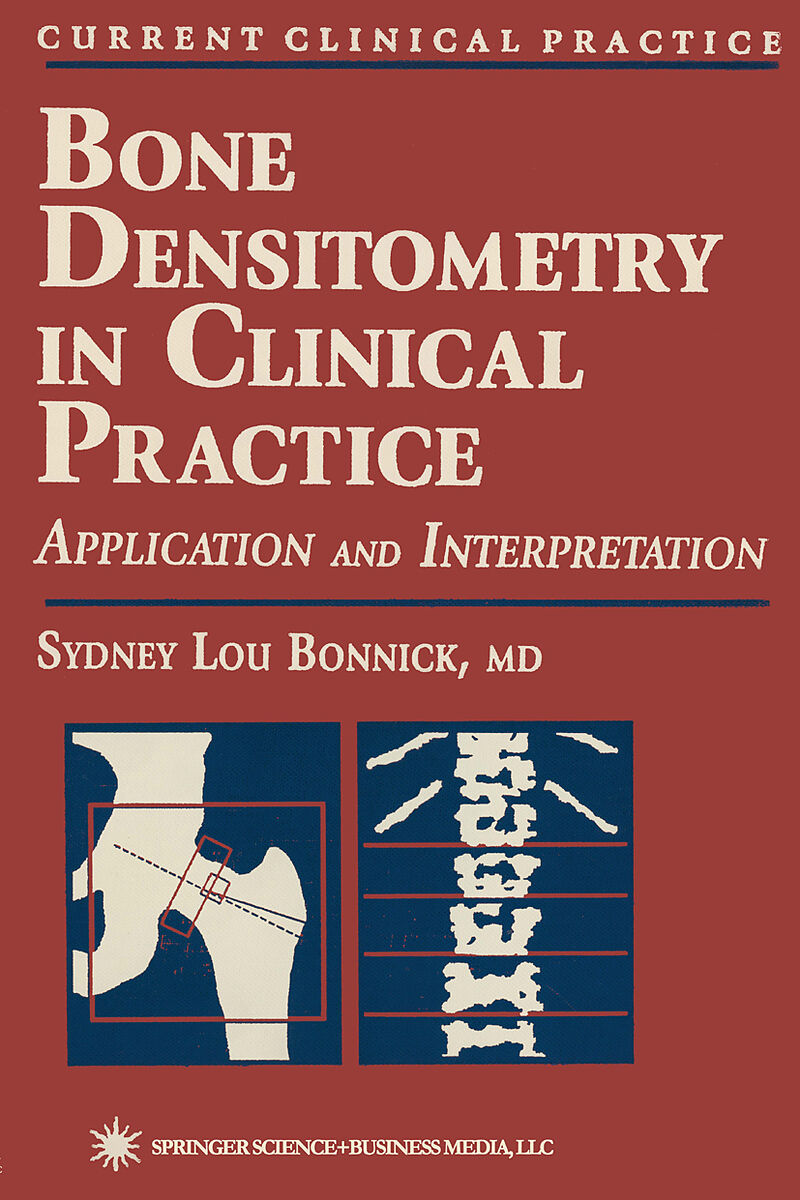
Bone Densitometry in Clinical Practice
Beschreibung
In Bone Densitometry in Clinical Practice, Dr. Sydney Bonnick summarizes the state-of-the-art in X-ray bone densitometry, highlighting for today's primary care physicians and densitometrists the expert application of densitometry techniques in patient managem...Format auswählen
- E-Book (pdf)CHF 106.90
Wird oft zusammen gekauft
Andere Kunden kauften auch
Beschreibung
In Bone Densitometry in Clinical Practice, Dr. Sydney Bonnick summarizes the state-of-the-art in X-ray bone densitometry, highlighting for today's primary care physicians and densitometrists the expert application of densitometry techniques in patient management. Dr. Bonnick describes the various densitometry techniques currently in use and how to intelligently select among them in a wide variety of clinical circumstances. She also shows how to interpret the computer-generated data and how to recognize and avoid interpetation pitfalls from the effects of artifacts and structural changes. Physicians performing densitometry will learn the key elements to include in a densitometry report to referring doctors, and how to gain mastery of the sophisticated quality control procedures necessary for the successful performance of bone densitometry.
Offering the most comprehensive but easily readable explanation of diagnostic densitometry for the primary care physician and technologist, Bone Densitometry in Clinical Practice is destined to become the essential guide for medical personnel working with densitometry. Its numerous illustrations, practical examples, and tables will prove invaluable to physicians, whether new to the field or considerably experienced in the everyday practice of densitometry.
Klappentext
Precision and accuracy are terms that are used in quantitative scientific fields to describe the reproducibility of a measurement or the capacity of a measurement to quantify the actual biological matter present. Precision and accuracy are also important applications in the quality control and quality assurance of the performance and interpretation of bone mass measure ments. Precision and accuracy also reflect the values and qualities of the author of this important text in the clinical application of bone densitometry. This is the first textbook of its kind devoted entirely to the proper use of this technology in the practice of medicine. Dr. Sydney L. Bonnick has devoted a majority of her career helping to define excellence in this exploding area and in doing so, has earned the respect and admiration of the international bone densitometry community. Confusion abounds in this field due to the proliferation of bone densito metry devices, including the various models that can measure many skel etal sites, the different normative data bases used, and the establishment of diagnostic categories of low bone mass. Dr. Bonnick's authoritative and carefully referenced text will certainly clarify and broaden the knowledge of those physicians who currently perform bone densitometry. This text is designed to be utilized by a wide range of medical specialists: endocrinolo gists, rheumatologists, gynecologists, radiologists, orthopedic surgeons, and nephrologists.
Inhalt
Chapter 1. Densitometry Techniques in Medicine Today. Plain Radiography in the Assessment of Bone Density. Qualitative Spinal Morphometry and the Singh Index. Qualitative Spinal Morphometry. The Singh Index. Quantitative Morphometric Techniques: Calcar Femorale Thickness, Radiogrammetry, and the Radiologic Osteoporosis Score. Calcar Femorale Thickness. Radiogrammetry. The Radiologic Osteoporosis Score. Radiographic Photodensitometry. Radiographic Absorptiometry (RA). Photon Absorptiometric Techniques. Single-Photon Absorptiometry (SPA). Dual-Photon Absorptiometry (DPA). Dual-Energy X-Ray Absorptiometry (DXA). Peripheral DXA Units. DTX-200. pDEXA. Peripheral Instantaneous X-Ray Imager (PIXI). Single-Energy X-Ray Absorptiometry (SXA). Quantitative Computed Tomography (QCT). Peripheral QCT. References. Chapter 2: Densitometric Anatomy. The Skeleton in Densitometry. Axial and Appendicular skeleton.Weight-Bearing and Non-Weight Bearing Skeleton. Central and Peripheral Skeleton. Skeletal Site Composition. The Spine in Densitometry. Vertebral Anatomy. Artifacts in AP Spine Densitometry. Vertebral Fractures. Effect of Osteophytes on BMD. Effect of Aortic Calcification on BMD. Effect of Facet Sclerosis on BMD. Other Causes of Artifacts in AP Spine Studies. The Spine in the Lateral Projection. The Proximal Femur in Densitometry. Proximal Femur Anatomy. Effect of Rotation on BMD in the Proximal Femur. Effect of Leg Dominance on BMD in the Proximal Femur. Effect of Artifacts on BMD in the Proximal Femur. The Forearm in Densitometry. Nomenclature. Effect of Arm Dominance on Forearm BMD. Effect of Artifacts on BMD in the Forearm. Other Skeletal Sites. References. Chapter 3. Statistics in Densitometry. Mean, Variance, and Standard Deviation. The Mean. Variance and Standard Deviation. Coefficient of Variation. Standard Scores. Z-Scores. T-Scores. Measures of Risk. Prevalence and Incidence. Prevalence. Incidence. Absolute, Relative, and Attributable Risk. Absolute Risk. Relative Risk. Attributable Risk. Odds Ratios. Confidence Intervals. Accuracy and Precision. Accuracy. Precision. Correlation. Statistical Significance and the P-Value. References. Chapter 4. The Importance of Precision in Densitometry. Performing a Short-Term Precision Study. Mathematical Procedures Used to Calculate Precision. Applying the Precision Value to the Interpretation of Serial Measurements. The Confidence Interval for the Change in BMD Between Two Measurements. Effect of Precision on the Timing of Repeat Measurements of BMD. References. Chapter 5. Quality-Control Procedures for Densitometry. Establishing a Baseline Value with the Phantom. Shewhart Rules and CUSUM Charts. Shewhart Rules. CUSUM Charts. Automated Quality Control Procedures. References. Chapter 6. The Prediction of Fracture Risk with Densitometry. Prevalence of Fracture at Different Levels of BMD. Fracture-Risk Prediction. Site-Specific and Global Fracture Risk Prediction. Relative-Risk Fracture Data. Global Fracture-Risk Prediction. Site-Specific Spine Fracture-Risk Prediction. Site-Specific Hip Fracture-Risk Prediction. Applying Relative-Risk Data in Clinical Practice. Lifetime Risk of Fracture. Remaining-Lifetime Fracture Probability. Fracture Threshold. Other Risk Assessments Derived from, or Combined with, Densitometry. Pre-Existing Fractures. Increasing Number of Low Bone-Mass Sites. Hip-Axis Length. References. Chapter 7. The Effects of Age, Disease, and Drugs on Bone Density. Age-Related Changes in Bone Density. Bone Density in Children. Bone Density in Premenopausal Women. Dissimilar BMDs Between Skeletal Sites at Peak and Prior to Menopause. Bone Density in Perimenopausal Women. Dissimilar Spine and Femoral BMD in Perimenopausal Women. Changes in Bone Density in Postmenopausal Women. Changes in Bone Density in Men. Diseases Known to Affect Bone Density. Acromegaly. Alcoholism. Amenorrhea. Hyperandrogenic Amenorrhea, Exercise-Induced Amenorrhea. Anorexia Nervosa. Cirrhosis. Diabetes. Insu